The role of NBCA-MS in Enterocutaneous Fistulas
Riccardo Muglia MD

GASTROINTESTINAL FISTULAS
They are abnormal communications between two epithelized surfaces. They are most commonly iatrogenic and can be caused by trauma, radiation, IBD, etc., but they can also be spontaneous (75%/25%). They can occur all along the gastrointestinal tract and they are classified based on their position within the tract.
Foregut Fistulas
- Esophageal fistulas are mainly related to congenital and postsurgical atresia repair. They can be treated surgically, through re-thoracotomy, however, this is a technically challenging procedure, associated with significant morbidity (re-fistulation rate of 10%-32%). Another option is to treat them with glue sealant: this approach involves an endoscopic occlusion with tissue adhesives, which is completely safe and highly effective, with a success rate of 46% to 100%, with 1.3 sessions attempts per patient
- Refractory gastric/duodenal fistulas of iatrogenic etiology can also be treated successfully with sealant, fibrin glue, clipping, metal stents, and biologic plugs. Reported success rate: 57% to 100%
- Pancreatic fistulas treated with sealant report a cumulative success rate of 67% to 100% and 1.2 sessions to definitively close the fistula
- Biliary fistulas report a cumulative success rate of 78% to 100% and 1.2 sessions to definitively close the fistula
Midgut Fistulas
- Jejunal or ileal postoperative fistulas are the most common. Cumulative success rate with repetitive glue treatment of 67% to 100% and 1.2 sessions to definitively close the fistula
- Spontaneous fistulas due to Crohn’s disease are more difficult to heal
Hindgut Fistulas
- Colorectal: postoperative – Crohn’s disease – rectal cancer. Success rate with adhesive glue: 100%
- Anorectal: glandular etiology. Success rate with adhesive glue: 68% to 95% and 1.2 sessions to definitively close the fistula. Overall complication rate: 1%
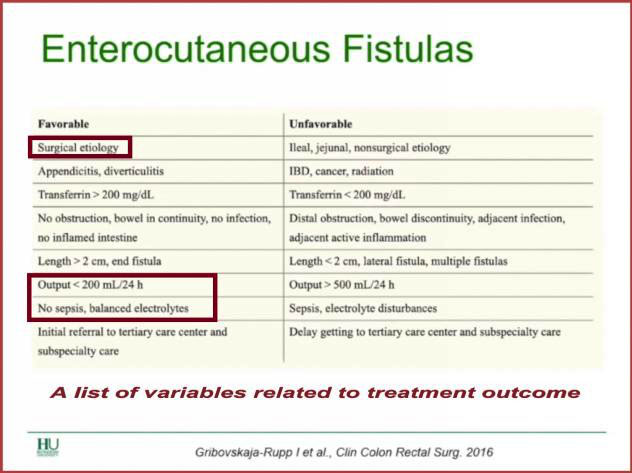
ENTEROCUTANEOUS FISTULAS
They are a particular kind of fistulas formed through an aberrant connection between a fistula in the Gl tract and skin/wound. They are classified in high output > 500 ml/24h and low output < 200 ml/24h and they are mostly iatrogenic (75-85%) with a low incidence of the spontaneous kind (15-25%), Another classification divides them in Type I (abdominal, esophageal, gastroduodenal), Type II (small bowel), Type III (large bowel), and Type IV (enteroatmospheric, regardless of origin).
MANAGEMENT
- Skin and Sepsi control is extremely important to manage enterocutaneous fistulas
- Nutrition translates into electrolytes requirements, usually provided in the crystalloid form
- Anatomy of the fistula needs to be thoroughly studied by means of CT or MRI scans
- Procedure:
1. Conservative treatment
i. Total parenteral nutrition to improve fluid and electrolyte balance and assure adequate nutritional support
ii. Empirical or targeted antibiotic therapy
iii. Somatostatin analogues: inhibitory effect on Gl secretions
iv. Low output fistula with no evidence of sepsis or localized infection: sealant glue
2. Image-guided drainage
i. Diagnostic: the injection of contrast medium through the drainage catheter may demonstrate communication with Gl lumen
ii. Therapeutic: removal of infected collection
3. Endoscopy
i. Clip: technology available for acute fistulas and perforations
ii. Plugs: more commonly used as an adjunct in the treatment of enteroatmospheric fistula
iii. Fibrin glue
4. Percutaneous treatments
5. Surgical repair
i. Definitive treatment but increased risk of morbidity
ii. Indication: no spontaneous closure by 12 weeks after sepsis control,
iii. nutritional optimization and wound care
iv. Success rates: 58 to 89%
v. Challenging dissections and possibility of recurrence
vi. 30-day morbidity rate: up to 82%
vii. Mortality rate: 2-5%
CYANOACRYLATE GLUE
- Obliteration of fistulous tracts
- Solidification of the compound within 30 seconds
- Induction of an inflammatory response that enhances fibrosis and foreign-body granuloma formation
- Ultimate epithelization
- Has to oppose to physiologic loads that tend to move tissues away from each other
- Must guarantee uniform distribution of the loads throughout the affected areas, without compromising the elastic properties of the natural tissues
CASE 1
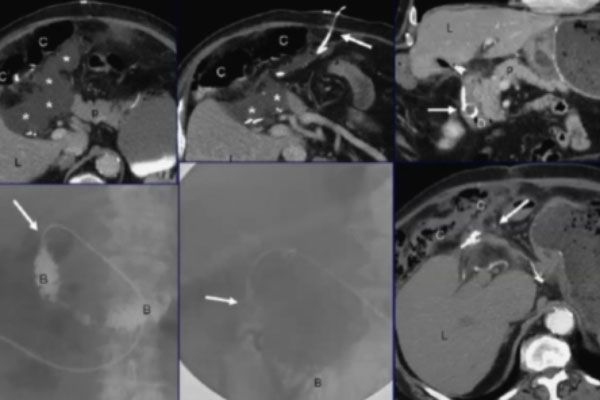
82 yo man, Gastric Resection for Gastric, Adenocarcinoma
After surgery, the patient presented with a collection positioned between transverse colon, liver, and pancreas, which we drained successfully and that disappeared after about 2 weeks. At 10-months follow up, though, we noticed the tip of the catheter inside the duodenum. We went into the lumen to retract the catheter and seal the fistula. The angiogram shows the radiopaque glue and no collection.
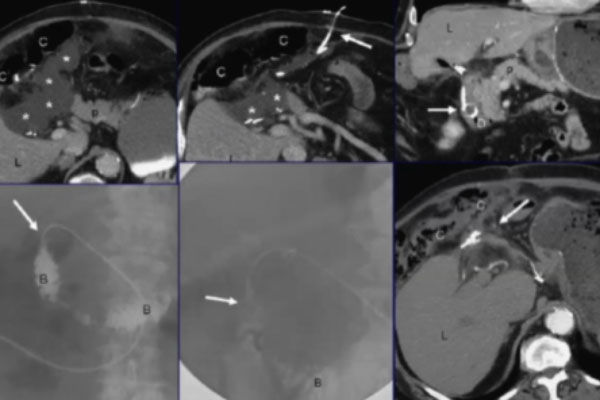
CASE 2
77 yo woman, Gastrectomy for Gastric Cancer
The patient had undergone surgical drainage, which we retraced by means of an angiographic catheter, detecting a fistula connected with the enteric lumen, behind the peritoneum. We used a hydrophilic guidewire to insert our catheter and sealed with a mix of Glubran 2 and Lipiodol, with successful results.
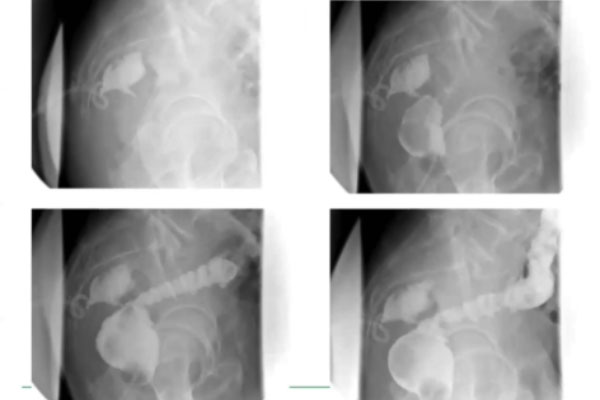
CASE 3
70 yo man, Anterior Resection for Rectal Cancer
This patient developed a collection behind the rectum. After draining it, we detected a fistula between the collection and the lumen of the rectum, which we treated with glue through the usual procedure. The picture shows the final result, which, as you can see, was extremely good.
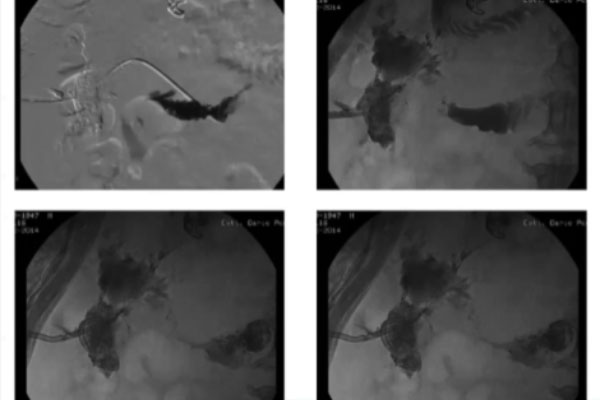
CASE 4
72 yo man, Duodenal Resection for Perforated Ulcer
This was an unfortunate case of a patient developing an extremely large collection of the right flank. We injected glue to seal the fistula but, unfortunately, the patient had to be treated multiple times as the fistula would not heal. The picture shows the impressive amount of glue we used over time to treat this case. The patient eventually had to undergo surgery to solve the problem. This goes to show that the occlusion of fistulas can be performed effectively by using glue, provided that the collection is not too large.




