Portal Vein Embolization – PVE
Felice D’Antuono MD
Over the past decades, perioperative care and surgical techniques improvement have led to an increased number of candidates for major liver resection. One of the limiting factors for surgery is the share of residual parenchyma, FLR (future liver remnant); in particular, high-risk patients for perioperative liver failure are those whose liver is removed:
>80% (HEALTHY LIVER)
>60% (CHRONIC HEPATOPATHY).
In literature, post-surgical liver failure reaches 30% and is still the leading cause of death after major liver resections. It appears directly related to FLR (future liver remnant).
Most surgical teams consider the minimum share of FLR / TLV as = 20%
However, FLR / TLV = 40% in case of chronic liver disease
FLR / TLV = 30% when CT is present in high doses
Preoperative Portal Embolization (PVE) is a technique developed to compensate for insufficient FLR volume by embolizing the portal branches of the parenchyma to be resected and direct the flow to the FLR branches.

Preoperative Portal Embolization (PVE) is a technique developed to compensate for insufficient FLR volume by embolizing the portal branches of the parenchyma to be resected and direct the flow to the FLR branches.
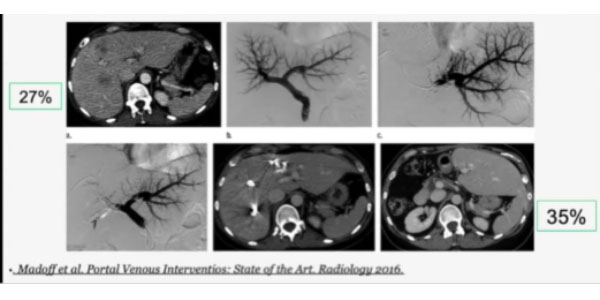
As an example, here is a successful case from literature: a patient with intrahepatic cholangiocarcinoma in the right lobe, who underwent extended right hepatectomy. sFLR/TLV starts at just 27% but a CT scan 2 weeks after right PVE shows hypertrophy with sFLR/TELV at 35%. PVE can be also used as a STRESS TEST: it is shown that a modest hypertrophic response to PVE is strongly correlated with postsurgical liver failure. In other words, an insufficient hypertrophic response can be considered an indicator of reduced regenerative capacity, and surgery should be avoided.
Liver regeneration properties have been well known since ancient Greece. In the 1920s, two French surgeons studying rabbit liver demonstrated that the ligation of the right lobe induced its atrophy while causing hypertrophy of the left one.
Today we know why that is: PVE triggers a membrane-and-cytoplasmic signaling cascade and the production of growth factors and cytokines, which increase the mitotic activity of the liver, thus causing its hyperplasia.
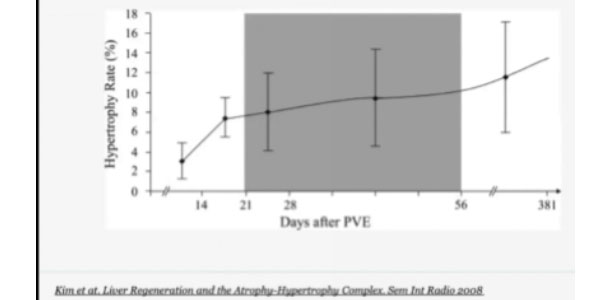
This answer is generally very rapid: the graph on the left shows a fast-growing hypertrophy rate over the first two weeks and the subsequent plateau phase. During this phase, CT scans are performed to evaluate liver volume in order to assess patient fitness for surgery.
PVE PROCEDURE
Percutaneous transhepatic approach has become the standard choice (a trans-ileocolic approach is also an option)
- Broad-spectrum antibiotic prophylaxis
- Procedure most frequently performed with local anesthesia and analgo-sedation
- Preliminary CT study to evaluate vascular anatomy – procedure planning is a crucial step
PV ANATOMY & APPROACH
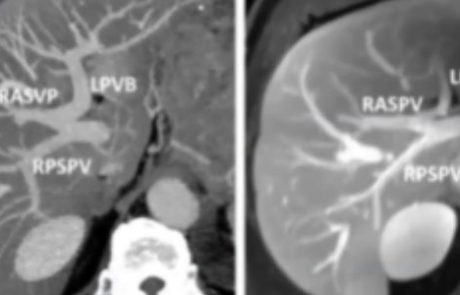
As standard anatomy can only be observed in about 30% of patients, we need to assess the case at hand before performing a portography. The picture shows an example of Type 3 or “Z” anomaly, where the left PV and the right anterior PV share a common trunk. If we approach the procedure with this information we can plan a selective categorization of the branches and perform a fast and safe embolization using glue, as in this case. In order to reduce the risk of later FLR-related problems such as thrombosis, dissection, or hematoma, we usually prefer ipsilateral access, however, studies have shown that a contralateral approach presents a similar kind and rate of possible complications. At any rate, it is very important to avoid lesions, to reduce the risk of dissemination and subcapsular hematoma.
A safe puncture technique is extremely important: we use ultrasound guidance with a 21/22 gauge Chiba needle to puncture a peripheral PV (usually segment 5/6), then we place a 4/5 Fr vascular sheath and proceed to do a preliminary portography before we advance our diagnostic catheter. Multiple projections (anterior, posterior, oblique) are needed to confirm vascular anatomy and plan the embolization, which must include the branches of S4 whenever surgical planning involves its resection. Cone-beam CT is also an option: the anatomic details are excellent and we can obtain a volumetric 3D reconstruction. After thorough and correct planning, we can proceed to select the vessels and insert a coaxial catheter. Another option is to exploit the venous flow to treat multiple branches at the same time.
EMBOLIC AGENTS
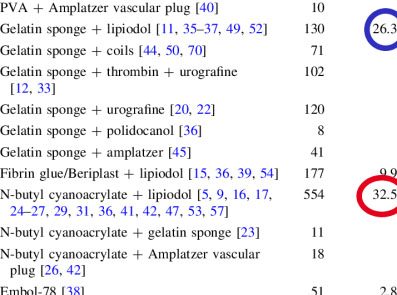
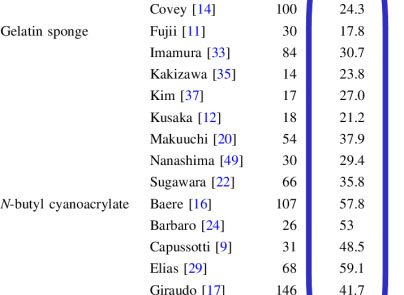
Although in this setting, we have tested all the embolic agents currently available in our interventional radiology department, from this systematic review we can clearly see the advantages of using glue from an FLR increase perspective.
van Lienden KP, van den Esschert JW, de Graaf W, et al. Portal vein embolization before liver resection: a systematic review. Cardiovasc Intervent Radiol. 2013;36(1):25-34. doi:10.1007/s00270-012-0440-y
From researches comparing different embolic agents we can gather more results, like those emerging from a 1996 study by De Baere, run on 31 patients, which reports:
“Hypertrophy of the FRL was 90% +/- 52% after 30 days with cyanoacrylate, 53% +/- 6% after 43 days with Gelfoam, and 44% +/- 30% after 35 days with coils.”
de Baere T, Roche A, Elias D, Lasser P, Lagrange C, Bousson V.Preoperative portal vein embolization for extension of hepatectomy indications. Hepatology. 1996;24(6):1386-1391. doi:10.1053/jhep.1996.v24.pm0008938166
Another interesting study by De Baere was run on animals in 2009 and compared embolized and non-embolized liver ratio. Glue and small PVA gave the best response:
Hydrophilic gel vs NBCA vs small PVA vs large PVA
N=2O pigs – left and median PVE (5 for each embolic agent)
Embolized liver /Non-embolized liver
- – Hydrophilic gel = 1.65
- – NBCA = 2.19
- – PVA 50 -150 = 1.57
de Baere T, Denys A, Paradis V. Comparison of four embolic materials for portal vein embolization: experimental study in pigs. Eur Radiol. 2009;19(6):1435-1442. doi:10.1007/s00330-008-1277-2
Another interesting study in the clinical setting which does not only show a higher FLR increase with NBCA but also a lower volume of the iodinated contrast used during the procedure:
NBCA vs Spherical Microparticles + Coils
N=34 (NBCA 20; SM + COILS 14)
FLR increase after 1 month
– NBCA = 74%± 69%
– SM + COILS = 23% 土 14%
Contrast Medium used
– NBCA = 162 ± 24 ml
– SM + COILS = 264 ± 43 ml
Guiu B, Bize P, Gunthern D, Demartines N, Halkic N, Denys A. Portal vein embolization before right hepatectomy: improved results using n-butyl-cyanoacrylate compared to microparticles plus coils. Cardiovasc Intervent Radiol. 2013;36(5):1306-1312. doi:10.1007/s00270-013-0565-7
This comparative study on NBCA vs Ethanol, while showing little difference in hypertrophic stimulus, reported a higher rate of major adverse events in patients treated with ethanol:
NBCA vs Absolute Ethanol
N=61 (NBCA 34; Ethanol 27)
NELV increase after 1 month
– NBCA = 116 ml
– Ethanol = 129.4 ml
ELV decrease after 1 month
– NBCA = 99.2 ml
– Ethanol = 191.9 ml
Sugawara S, Arai Y, Sone M, et al. Retrospective Comparative Study of Absolute Ethanol with N-Butyl-2-Cyanoacrylate in Percutaneous Portal Vein Embolization. J Vasc Interv Radiol. 2019;30(8):1215-1222. doi:10.1016/j.jvir.2018.12.020
A 2018 systematic review and meta-analysis aimed at evaluating the safety and effectiveness of NBCA in PVE, reported the following data:
“The literature search yielded 18 relevant articles. Six hundred and seven patients (383 men, 220 women; mean age 60.7 years) with procedures describing PVE utilizing NBCA were reviewed. The most common underlying hepatic malignancies were colorectal metastases (n = 348), followed by cholangiocarcinoma (n = 92), and hepatocellular carcinomas (n = 89).
Technical success was reportedly achieved in 603/607 patients, for a success rate of 99.3%. Fixed effects meta-analysis of the relative hypertrophy rate of the FLR among studies resulted in an aggregate rate of 49.4 ± 1.3%. Of the patients who underwent attempted PVE, 461/607 (75.9%) eventually underwent surgical resection. Major complications following PVE occurred in 19 patients (3.13%), while minor complications following PVE occurred in 38 patients (6.26%).”
Wajswol E, Jazmati T, Contractor S, Kumar A. Portal Vein Embolization Utilizing N-Butyl Cyanoacrylate for Contralateral Lobe Hypertrophy Prior to Liver Resection: A Systematic Review and Meta-Analysis [published correction appears in Cardiovasc Intervent Radiol. 2018 Nov;41(11):1811]. Cardiovasc Intervent Radiol. 2018;41(9):1302-1312. doi:10.1007/s00270-018-1964-6