Bland Embolization: NBCA in Hepatocellular Carcinoma HCC
Vittorio Pedicini MD
As we all know, bland embolization is the best treatment for HCC: our goal, in this case, is to induce ischemic damage to the tumor. This is also done by means of Transarterial Chemoembolization (TACE), a treatment that delivers the drugs, through a blood vessel, straight into the tumor.
As of today, though, no evidence suggests that TACE is more effective than simple embolization (TAE).
Pertaining literature started with a 2002 paper published on The Lancet. This was a randomized study run by the Barcelona-Clinic team on 112 patients, divided into three groups and assigning 37 pts to TAE (gelatin sponge), 40 to TACE (gelatin sponge plus doxorubicin) and 35 to control treatment. While the resulting interpretation was that “Chemoembolisation improved survival of stringently selected patients with unresectable hepatocellular carcinoma,” the difference between TACE and TAE appeared insignificant.
Llovet JM, Real MI, Montaña X, et al. Arterial embolisation or chemoembolisation versus symptomatic treatment in patients with unresectable hepatocellular carcinoma: a randomised controlled trial. Lancet. 2002;359(9319):1734-1739. doi:10.1016/S0140-6736(02)08649-X
Several pieces of research followed suit, and the validity of chemoembolization as a treatment for HCC has been well established since. However, as far as optimal schedules are concerned, or whether embolization alone can yield the same results, the data is yet inconclusive.
A 2007 systematic review was conducted to delve into the topic, using additional elements such as PVA particles. The research concluded that: “No chemotherapeutic agent appears better than any other. There is no evidence for benefit with Lipiodol. Gelatin sponge is the most used embolic agent, but PVA particles may be better. TAE appears as effective as TACE. New strategies to reduce the risk of post-TACE complications are required.”
Marelli L, Stigliano R, Triantos C, et al. Transarterial therapy for hepatocellular carcinoma: which technique is more effective? A systematic review of cohort and randomized studies. Cardiovasc Intervent Radiol. 2007;30(1):6-25. doi:10.1007/s00270-006-0062-3
The PRECISION V study, run by Professor Johannes Lammer, Medical University of Vienna, in 2009, aimed at investigating the safety and efficacy of chemoembolization with DC Bead loaded with doxorubicin (PRECISION TACE with DC Bead). The results were extremely positive but might have been affected by the size of the particles employed for the embolization.
Lammer J, Malagari K, Vogl T, et al. Prospective randomized study of doxorubicin-eluting-bead embolization in the treatment of hepatocellular carcinoma: results of the PRECISION V study. Cardiovasc Intervent Radiol. 2010;33(1):41-52. doi:10.1007/s00270-009-9711-7
In fact, due to the liver’s unique dual blood supply, the smaller the particles, the stronger the ischemic effect: the optimal strategy could be to disrupt vascularization where the portal vein and hepatic artery converge, at the sinusoids – which we know are about 10–15 m in diameter. When you use particles that can fit this size, you can achieve impressive results in terms of ischemia and consequent effects on your target lesion.
This was the theory at the base of a study that our team ran on >50 pts in 2009, whose purpose was ”to report on the feasibility, local response, and 1-year clinical outcome of bland transarterial embolization (TAE) with 40 and 100 mm Embozene microspheres in patients affected by unresectable hepatocellular carcinoma (HCC).”
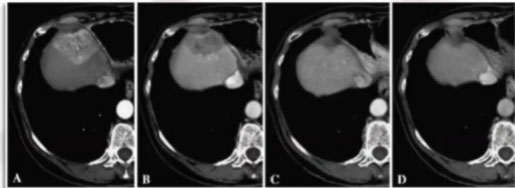
Local control results were extremely positive: in the picture, we can observe a case treated over a 12-month period, showing progressive lesion shrinking and eventually complete response.
At the time, local results were assessed according to RECIST criteria. The complete response rate might be higher today, using mRECIST criteria.
Bonomo G, Pedicini V, Monfardini L, et al. Bland embolization in patients withunresectable hepatocellular carcinoma using precise, tightly size-calibrated, anti-inflammatory microparticles: first clinical experience and one-year follow-up. Cardiovasc Intervent Radiol. 2010;33(3):552-559. doi:10.1007/s00270-009-9752-y
In 2016, a randomized trial was run by the Memorial Sloan Kettering Cancer Center to compare “the outcome of embolization using microspheres alone with chemoembolization using doxorubicin-eluting microspheres.” The study concluded that “there was no apparent difference between the treatment arms. These results challenge the use of doxorubicin-eluting beads for chemoembolization of HCC.”
Brown KT, Do RK, Gonen M, et al. Randomized Trial of Hepatic Artery Embolization for Hepatocellular Carcinoma Using Doxorubicin-Eluting Microspheres Compared With Embolization With Microspheres Alone. J Clin Oncol. 2016;34(17):2046-2053. doi:10.1200/JCO.2015.64.0821
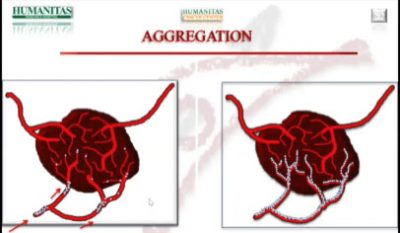
It was around this time that we started to employ Glubran®2 in our treatments. When we inject the particles in the arterial flow, we aim at ideal distribution, which sometimes fails to happen due to the aggregation of the particles in the vessel. This aggregation usually occurs in the proximal side of the artery, and, when it does, the distal bed is difficult to reach.
Probably due to this phenomenon, sometimes the contrast media will stop in the arterial flow and then start to revascularize after a few minutes. We can hope for the systolic pressure to do its job, and push the particles into place, but we cannot be sure.
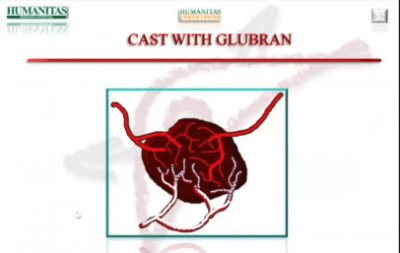
This heterogeneous distribution could very likely affect the patient response, as the difference between complete and partial response might well depend on lesion coverage. Reinforcing our treatment with glue helps us to obtain the perfect embolization of our target.
CASE 2 – CAPSULATED HCC
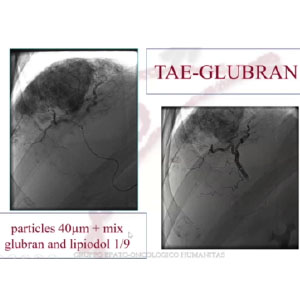
In this case we had a capsulated, partially exophytic lesion, which we treated with TAE-Glubran®2 (1:9 ratio).
In the picture, we can see the embolization, with the same characteristics as the previous case. 3 months later, we could observe a complete devascularization of the lesion.
CASE 3 – Adrenal Mass Bleeding
77 yo man with chronic hepatitis (esotoxic) Varices F2, AFP 800
This case presented a small HCC lesion on segment 8, which we embolized selectively, first with particles and then with glue. We could notice some non-target embolization in another small vessel, with ischemic damage of the dorsal territory. At follow-up, 1 month later, control showed a lesion without vascularization.
In January 2020, we published our “Survival analysis of 230 patients with unresectable hepatocellular carcinoma treated with bland transarterial embolization”, describing our experience with TAE on HCC patients over a period of 7 years. We reported high survival rates of 85% at 1-year and 59% at 2-years. These results are in line with comparative literature on chemoembolization, however, no clinical trial with the same number of patients bore such high figures.
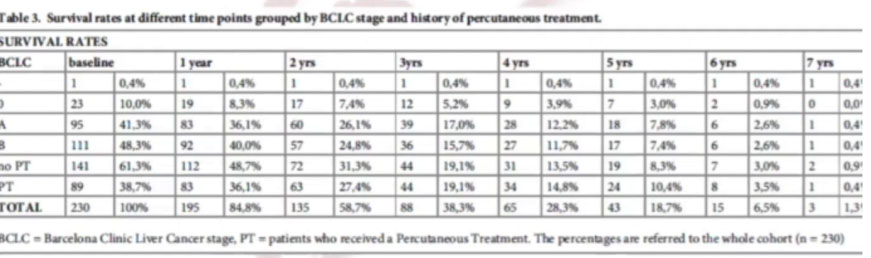
Lanza E, Muglia R, Bolengo I, et al. Survival analysis of 230 patients with unresectable hepatocellular carcinoma treated with bland transarterial embolization. PLoS One. 2020;15(1):e0227711. Published 2020 Jan 14. doi:10.1371/journal.pone.0227711